Diabetes
Diabetes at Torkard Hill
Patients with type 2 diabetes are looked after by the practice multidisciplinary team; lead by our fantastic nursing team who have undertaken additional training in diabetes, with input from your GP and diabetes nurse specialists.
Patients with type 1 diabetes are usually managed by the hospital diabetes team.
What is type 2 diabetes?
Type 2 diabetes is a common condition that results in high sugar (glucose) in the blood. It can cause a variety of symptoms including thirst, frequent urination, and tiredness. Left untreated, it can damage your eyes, heart, kidneys and nerves.
It is a lifelong condition.
We can treat it - you will need change your lifestyle and diet, may need to take medicines, and have regular check-ups at our practice.
Diagnosing and monitoring diabetes
How is diabetes diagnosed?
If you have symptoms of diabetes, we would organise a blood test to check your sugar levels. This may need to be repeated again, if abnormal, to be sure.
How often is my sugar checked?
We would usually check your bloods to monitor your sugar control every 6 months, and, depending on the severity, invite you for a full review every 12 months, or sooner.
What do you check at my annual review?
In addition to blood tests, your review includes measuring your weight, height and blood pressure. We will also ask for a urine sample, that tests for any unusual protein – this is another way of checking your kidneys are working well. We will also examine your feet to check the pulses and sensation.
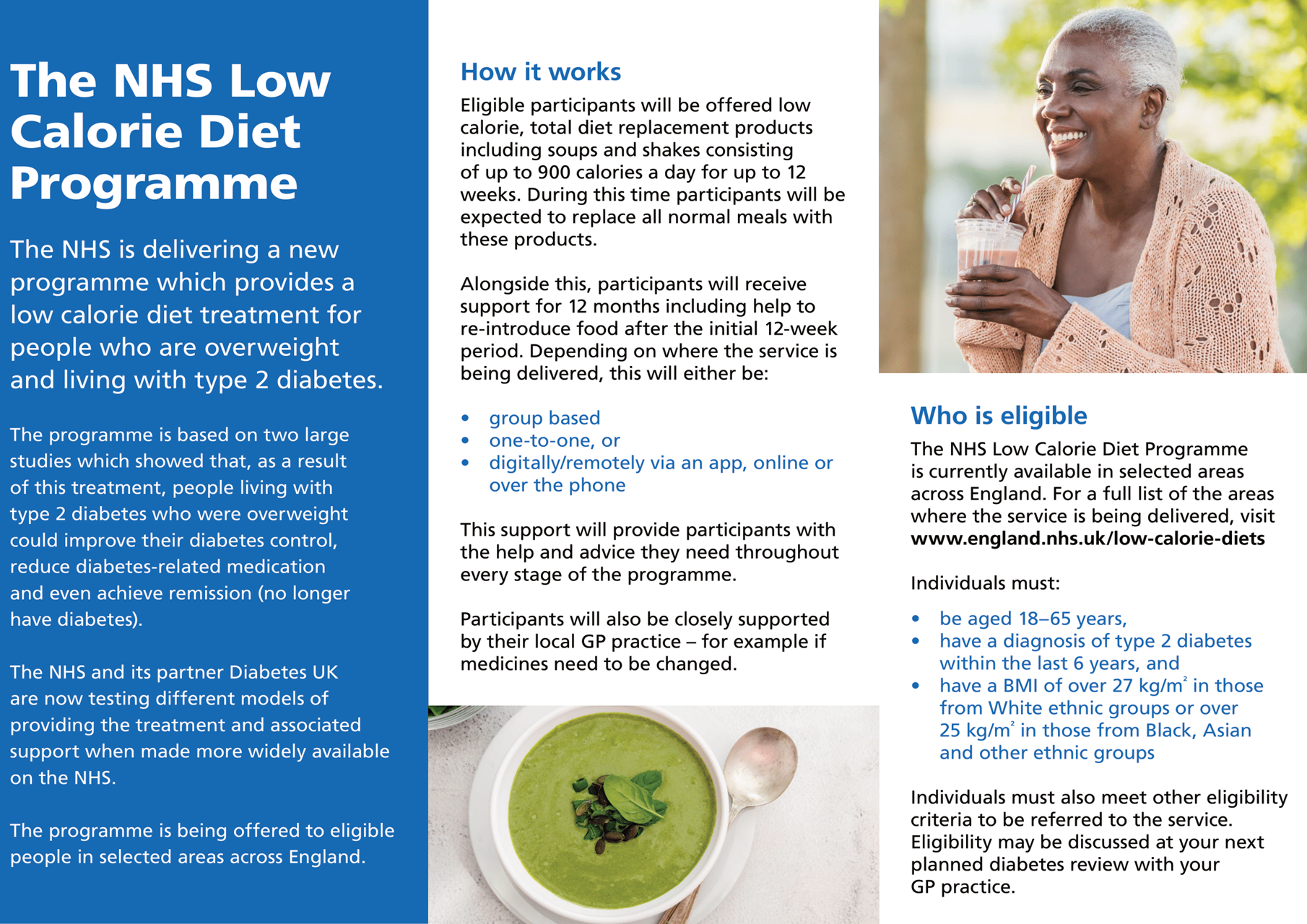
Diabetic eye screening
Diabetes can affect your vision, therefore to pick up any early signs of eye disease, you will be offered an eye screening appointment each year. A picture of the back of the eyes is taken, to check for any damage, called “retinopathy”.
This is arranged by Nottingham University Hospitals.
Blood tests – what do they mean?
HbA1c – Glycosylated haemoglobin is your average blood sugar levels for the previous 2-3 months. It is a very useful way of checking your sugar control and we use this to adjust your treatment. We would aim a level of less than 52.
Lipids – cholesterol is very important in diabetes. It is another risk for developing complications associated with diabetes (eg heart and stroke disease). Often, if you have diabetes, you may also have high cholesterol. We would aim to keep your total cholesterol below 4.
UEs – Urea and electrolytes are very important to check how well your kidneys are working; we know diabetes can affect your kidney function. We check the “eGFR” and this should be over 60%.

Treatment of diabetes
The aim of treatment is to reduce your sugars to a safer level. Ideally your HbA1c should be below 52.
Lifestyle changes are essential to reduce sugar levels, and for some, this may be the only treatment necessary. There are many helpful resources you can use to reduce your sugar intake; our nurses can advise you on this when you are diagnosed, or at your annual reviews.
We would strongly recommend signing up to attend a DESMOND programme (see below).
You should also download the free “Change4Life Food Scanner” app on your smartphone; this is an easy way of finding out how much sugar is in your favourite food and drink! Another we recommend is "Carbs & Cals" - see below!
If we need to prescribe you medication, there are a number of options that include tablets and injections, depending on the severity of your diabetes, and any other health problems you may have. More information about medication can be found here .
Healthy Living

DESMOND
DEMOND stands for “Diabetes Education Self-Management for Ongoing and Newly-Diagnosed”.
It is a fantastic, free, group education programme that anyone in Nottinghamshire, with Type 2 Diabetes, can sign up to. Attending this programme has a positive impact on how well your diabetes is treated.
- The aims of the DESMOND programme:
- Thoughts and feelings of the participants around diabetes
- Understanding diabetes and glucose: what happens in the body
- Understanding more about monitoring and medication
- Understanding the risk factors and complications associated with diabetes
- How to take control – Food Choices – Physical Activity
- Planning for the future
To self refer, call 01623 484837 or email desmondreferrals@nottshc.nhs.uk
Get the free Food Scanner app
Download the Change4Life Food Scanner app to bring labels to life and find out what's really in the food and drink you're buying.
Download the app:
Carbs & Cals
Carbs and Cals is an award winning app and book, recommended by Diabetes UK. We have a number of patients who recommend this, to reduce their calories and sugars.
Take a look at www.carbsandcals.com
Download the app:
Foot care
Foot care for diabetics is incredibly important because foot related complications are more common, and can develop complications.
Diabetes can affect your circulation and sensation, leading to problems such as ulcers, pain and even serious infections.
This leaflet has helpful advice about to look after your feet: Foot Care.pdf
If you develop any open areas, such as sores, to your feet, please contact the surgery as soon as possible to see one of our practice nurses.

Other information
Glucose meters
If you have erratic sugar control, or take certain diabetes medications, you may be prescribed a glucose meter, allowing you to test your sugar levels.
What happens if I am unwell? Your “sick day rules”
If you are unwell, for example you have an infection, sickness or diarrhoea, it is important to keep hydrated and ensure you eat adequate amounts of carbohydrate and protein; avoid starving yourself.
Your medications may need to be reduced or suspended until the illness recovers and you feel well again.
Your diabetes nurse will be able to advise you about this at your annual review, and, of course, if you have an illness that doesn’t seem to be settling, please ensure you speak to the emergency doctor at the practice, who will be available every weekday.
You can find more information and download a leaflet here
Insulin and injections
People often worry that diabetes means lifelong injections. Thankfully, diabetes treatment has been transformed over the past few years, and only a minority need injections of insulin. There are many more treatments including a variety of tablets that can be taken orally.
Freestyle Libre
You may have heard of a sugar monitoring system called “Freestyle Libre”; this is not usually prescribed for patients with Type 2 diabetes, unless you have very severe disease and are treated by a specialist diabetes doctor.
Can I still drive if I have diabetes?
Yes – most patients with diabetes can still drive, if they have good control, no hypos, and you feel well. You may need to monitor your sugar levels with a meter in some cases. More information can be found at: https://www.diabetes.org.uk/guide-to-diabetes/life-with-diabetes/driving and https://www.gov.uk/government/publications/information-for-drivers-with-diabetes
Patients with a new diagnosis
Please take a look at this patient information leaflet!
Pre-diabetes
In pre-diabetes, your blood sugars are raised, however not so high that you have type 2 diabetes. An HbA1c of 42-47 inclusive is pre-diabetes.
You are at increased risk of developing type 2 diabetes when you have pre-diabetes.
Around 1 in 4 people with pre-diabetes will develop diabetes within ten years.
The lifestyle changes we recommend for those with diabetes (see above) are recommended to treat pre-diabetes.
Useful links and information leaflets to download
- Dietary information including meal plans: https://www.diabetes.org.uk/guide-to-diabetes/enjoy-food/eating-with-diabetes
- More information about medication: https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/treating-your-diabetes/tablets-and-medication
- Ramadan and diabetes: https://www.diabetes.org.uk/guide-to-diabetes/managing-your-diabetes/ramadan
Page created: 13 July 2020