Covid-19
Due to the rapidly changing picture of Covid, the information on this page will be regulary updated as guidelines change.
Last Updated 11/07/2024.
Covid 19 treatment for those at highest risk
PANORAMIC Study
Have you tested positive for COVID-19 and experiencing COVID-19 symptoms, starting in the last 5 days? The PANORAMIC Trial aims to find antiviral treatments to improve symptoms and reduce hospital admissions for people with COVID-19.
Eligibility for PANORAMIC study
• All patients aged 50 or over, OR
• Patients aged 18-49 with one of the following:
▪ Chronic respiratory disease (including chronic obstructive pulmonary disease (COPD), cystic fibrosis and asthma requiring at least daily use of preventative and/or reliever medication)
▪ Chronic heart or vascular disease
▪ Chronic kidney disease
▪ Chronic liver disease
▪ Chronic neurological disease (including dementia, stroke, epilepsy)
▪ Severe and profound learning disability
▪ Down’s syndrome
▪ Diabetes mellitus (Type I or Type II)
▪ Immunosuppression: primary (e.g. Inherited immune disorders resulting from genetic mutations, usually present at birth and diagnosed in childhood) or Secondary due to disease or treatment (e.g. sickle cell, HIV, cancer, chemotherapy)
▪ Solid organ, bone marrow and stem cell transplant recipients
▪ Morbid obesity (BMI >35)
▪ Severe mental illness
▪ Care home resident
▪ Considered by recruiting clinician to be clinically vulnerable
Visit: www.panoramictrial.org/
Covid 19 Frequently Asked Questions (FAQ)
Q: I have a cough but no fever or changes in smell or taste – it can’t be Covid-19, can it?
A: The current guidelines are ANY of persistent cough OR fever OR change smell/taste. You do not have to have all three.
Q: Why do I have to stay at home? I feel fine otherwise!
A: Staying at home is the ONLY way to stop the spread, and avoid infecting others – some of whom may not be fortunate to be able to clear the virus themselves.
Q: Is there a cure for Coronavirus?
A: At present, there is no cure for the virus. Treatment is supportive until you clear the virus. Antibiotics don’t treat viruses. The annual flu vaccine does not protect you from coronavirus. If you are in a risk group, you may need your oxygen levels monitoring, and may qualify for specialist treatment or trials (above).
Q: I have a number of health problems. My employer wants to know if I am at risk and what do I do with work?
A: It is your employer’s responsibility, not your GP, to make any relevant work related risk assessment. Employers should refer you to their occupational health teams if they are unsure.
Q: How do you know if my cough is Covid-19? It feels like my asthma, flu or common cold!
A: It is very difficult to tell, in both adults and children, if your cough or fever is related to Covid-19 or something else. We appreciate the consequences of needing to isolate and the difficulties getting a test, and often we are hearing patients trying to persuade themselves it’s something else - however the safest thing if unsure is to istay at home!
Q: I am medically exempt from wearing a face covering; do I need a letter from my GP?
A: You do NOT need a letter from your GP, and the practice will not be providing these. All the information about exemptions, including printing out your own cards, can be found at https://www.gov.uk/government/publications/face-coverings-when-to-wear-one-and-how-to-make-your-own/face-coverings-when-to-wear-one-and-how-to-make-your-own
Q: I have tested positive for Covid19 and have completed my isolation, but still feel unwell. What do I do?
A: We would ask you to ring the surgery so that the emergency doctor can speak to you about your ongoing symptoms. In addition, if you require further time off, we will also issue you with a sick note.
Q: I have covid infection but am due my vaccine, what should I do?
A: We recommend at least 28 days after the onset of your symptoms, before having your Covid vaccination.
Q: I am under the hospital, and due to Covid19, my appointments, tests and procedures have been cancelled. I am unhappy, what can I do?
A: We would ask you to first discuss your concerns with your responsible doctor at the hospital; you can contact them via their secretaries, and the details can be found on your clinic letters. If you do not feel your concerns have been answered, you may speak to the Patient Advice and Liaison Service (PALS) - each hospital has these and can be reached via the hospital switchboards. We do appreciate that the NHS has had to make incredibly difficult decisions during this pandemic, and only the hospital can prioritise your case where clinically necessary.
Supporting your recovery after COVID-19
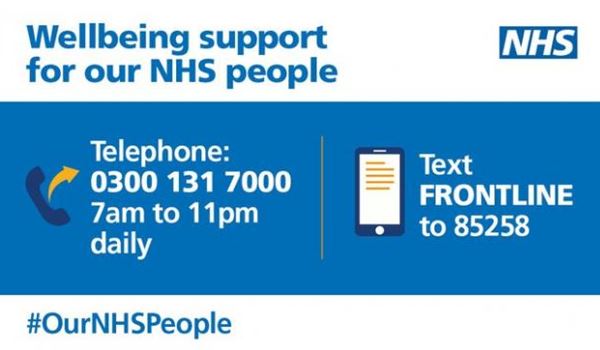
NHS Wellbeing Support
Our NHS People
We know some of our patients work within the NHS. There is specific support for frontline NHS staff at Our NHS People.
Take a look: https://people.nhs.uk/
Page created: 13 July 2020